Get to know our team on LinkedIN:
Lindsay Nease, Michael Cawthon, Lan Lan, Jayce Schwartz, Tyrell Snagg
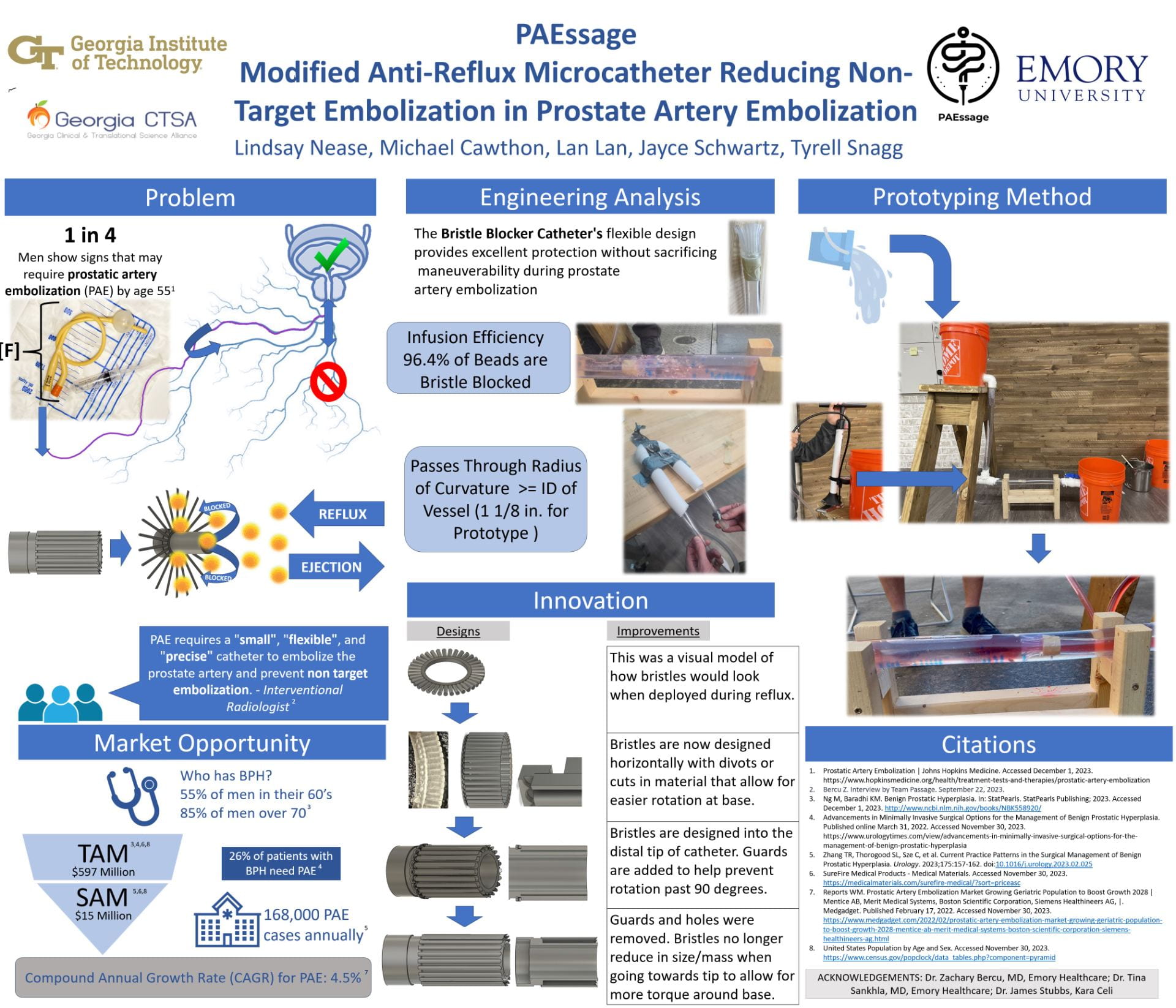
PAEssage
Modified Anti Reflux Micro-catheter That Prevents Off Targeting in Prostatic Artery Embolization
Project Description:
Prostate Artery Embolization (PAE) is a minimally invasive procedure utilizing a microcatheter to insert microspheres obstructing the blood supply to an enlarged prostate, thereby reducing its size. This technique is primarily used for benign prostatic hyperplasia (BPH) cases requiring surgical intervention. Annually, approximately 168,000 PAE procedures are conducted, with its demand growing at an annual compound rate of 4.5%. A significant challenge in PAE is non-target embolization, where microspheres unintentionally enter and affect adjacent tissues, leading to complications like ulcers, discoloration, and tissue death. Current anti-reflux microcatheters, designed to prevent this issue, are either too large for prostate vascular structures or do not have the maneuverability that is desired by interventional radiologists (IRs) to navigate the tortuous anatomy common in older men.
To enhance PAE’s safety, we have developed an innovative microcatheter featuring bendable rod like appendages, bristles, at its tip to capture any refluxed microspheres while having less effect on its maneuverability. Our prototype, tested under simulated blood flow conditions at enlarged scale, successfully trapped refluxed spheres, demonstrating its potential efficacy. Although the prototype is larger than actual anatomical scale, significant efforts were made to demonstrate equivalence, and it lays the groundwork for addressing PAE risks. Moving forward, we aim to produce a life-sized model and conduct comprehensive in vitro testing to validate its safety and effectiveness.